The Neuromuscular Junction
Normal NMJ Physiology
It is important to have at least a basic understanding of normal neuro-muscular junction physiology so that you can explain
- How non-depolarising muscle relaxants work
- How depolarising muscle relaxants work
- Why fade and post-tetanic facilitation occur
Sequence of Events Leading to Muscle Contraction
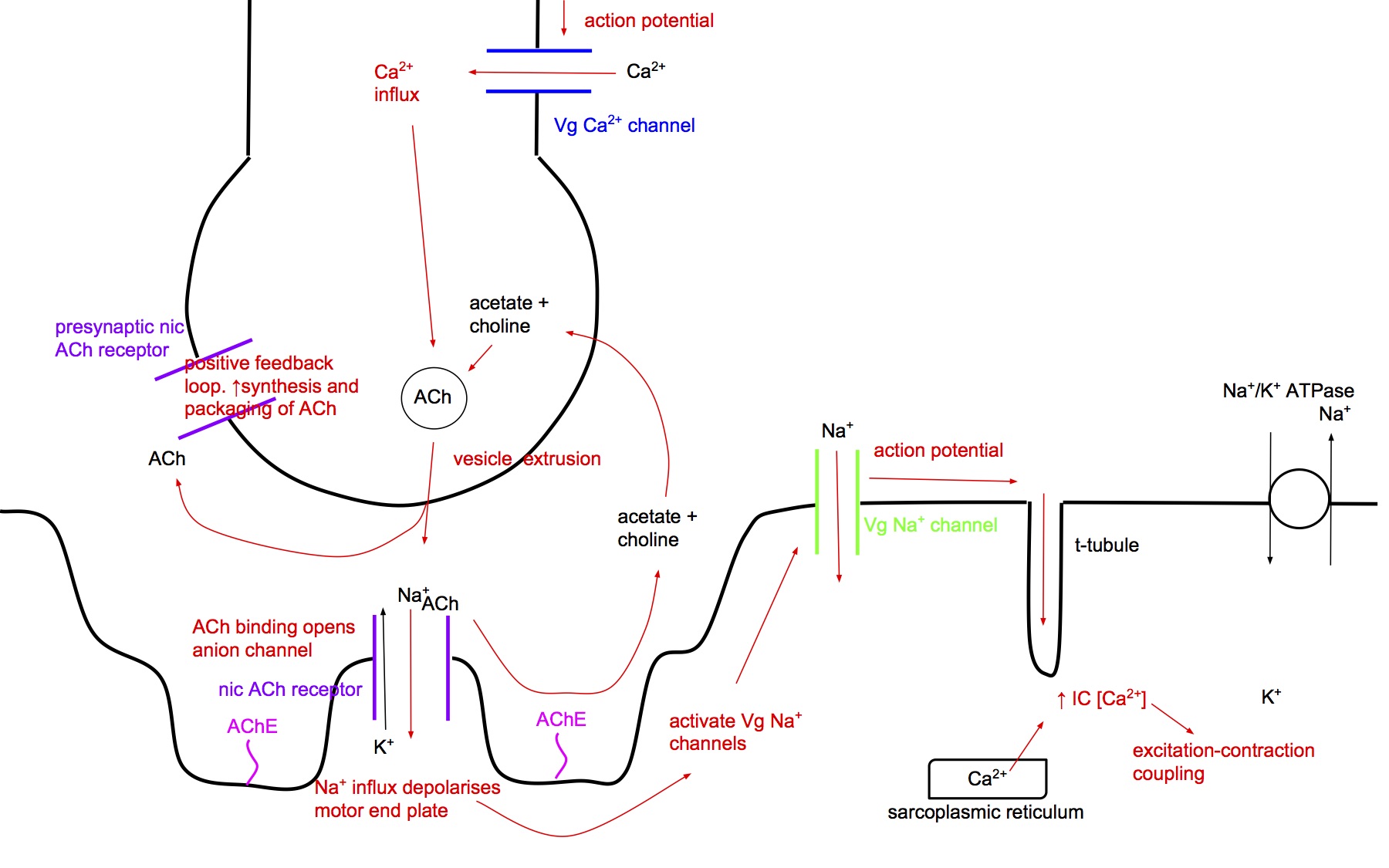
- Action potential down nerve fibre to nerve terminal (wave of depolarisation spread by voltage-gated sodium channels in the cell membrane)
- Opens voltage-gated Ca2+ channels at the nerve terminal
- Influx of Ca2+ → release of acetylcholine (ACh) containing vesicles into the synaptic cleft
- ACh diffuses across the synaptic cleft and binds to nicotinic ACh receptors in the motor end plate (the area of muscle fibre that synapses with the nerve fibre). (It's called a plate because it has a flat dinner plate shape)
- The nic ACh receptor is a ligand-gated cation channel, and when activated it opens up, allow influx of Na+ (and efflux of K+) down their concentration gradients → depolarises the motor end plate
- The depolarisation associated with the release of a single vesicle of ACh is called a miniature end plate potential (MEPP). The summation of all the MEPPs is called the end plate potential (EPP)
- When the EPP depolarises past the threshold for activation of the surrounding voltage-gated Na+ channels → action potential along the muscle fibre cell membrane
- AP is propagated down the t-tubule system → release of Ca2+ from sarcoplasmic reticulum
- ↑ intracellular [Ca2+] → excitation-contraction coupling (you need to read up a bit on that process)
Simultaneous Events
- Presynaptic positive feedback loop
- ACh released into the synaptic cleft also binds to pre-synaptic nic ACh receptors → accelerates the resynthesis of ACh and packaging into vesicles (this is important for explaining fade)
- Resetting the system
- ACh in the synaptic cleft is rapidly broken down by acetylcholine esterase (AChE) - an enzyme which is tethered to the post-synaptic membrane and also free floating in the synaptic cleft - to choline and acetate, which are taken up by the nerve terminal and resynthesised into ACh
- In fact, a large proportion of the released ACh is broken down before it even reaches the post-synaptic ACh receptors
- The cation channel of the nic ACh receptor closes
- The Na+/K+ ATPase pumps out the excess Na+ and returns the membrane potential back to baseline
- This repolarises the cell membrane and cycles the Vg Na+ channels from the inactivated to the resting state
- The NMJ is now ready to respond to the next nerve stimulus
Key Points to Understand
- Transmission of the electrical signal across the NMJ is a high fidelity system, ie an action potential in the nerve fibre very reliably results in an action potential in the muscle fibre, leading to excitation-contraction coupling
- This is because there is a high margin of safety built into the system
- Excess ACh released. The amount of acetyl choline released pre-synaptically by the nerve ending with each stimulus is far in excess of what is required to activate enough post-synaptic nACh receptors such that the membrane potential depolarises to reach the threshold of the voltage-gated sodium channels and propagate the action potential down the muscle fibre
- Excess number of ACh receptors. The number of nACh receptors at the motor end plate greatly exceeds the minimum number needed to be able to depolarise to threshold – 70% can be blocked without impairing transmission
- With high frequency nerve stimulation, for each consecutive nerve impulse, slightly less ACh is released pre-synaptically as there is insufficient time to resynthesise and repackage the ACh into the vesicles. However, transmission of the signal is not hampered because of the aforementioned reasons
- Don't confuse the EPP, which is due to nic ACh receptors in the motor end plate, with the AP, which is due to Vg-Na+ channels surrounding the motor end plate. This is where most people get confused about how sux works
Non-Depolarising Muscle Relaxants
Mechanism of Action
- NDMRs act as competitive antagonists at the NMJ nicotinic ACh receptors (both post-synaptic and pre-synaptic)
Deep Paralysis
- If a NDMR is present at a high concentration in the NMJ, a high proportion of post-synaptic ACh receptors will be blocked, and even if ACh activates all the remaining receptors, the EPP is not enough to depolarise the membrane past the threshold of the Vg Na+ channels and the AP is not propagated
- No muscle fibres will contract in response to a nerve stimulus and the patient is deeply paralysed
Partial Paralysis
- At a lower concentration of NDMR, when roughly 70% of ACh receptors are blocked, there may be just enough ACh receptors available to be activated for the membrane to be depolarised past threshold and propagate the AP
- A small difference in the amount of ACh present in the synaptic cleft may make the difference between reaching threshold or not
- For an individual muscle fibre, whether it reaches threshold and contracts or not is an all or nothing event
- Around this critical concentration of NDMR, some motor units may reach threshold and contract, while others may not, ie only a proportion of the total number of muscle fibres contract, resulting in a reduced overall twitch strength
Fade
- In the presence of partial block due to NDMR, the safety margin for signal transmission is drastically reduced, for two reasons:
- NDMRs antagonise the pre-synaptic ACh receptors which are part of a positive feedback loop that stimulates the synthesis and packaging of ACh into vesicles. Hence with each subsequent stimulus, the decrease in the amount of ACh released is accentuated
- NDMRs block a high proportion of the post-synaptic ACh receptors
- Hence with each consecutive stimulus, such as from a Train-of-Four test, less and less motor units will reach threshold and contract, resulting in progressively decreasing summated twitch strength
Post Tetanic Facilitation
- A high frequency of nerve stimulation, such as from tetanus, results in a large amount of ACh being released into the synaptic cleft
- The ACh bind to and activate a large number of pre-synaptic nic ACh receptors
- This initiates a positive feedback loop whereby the synthesis and packaging of ACh into vesicles in the nerve terminal is accelerated
- For a short period of time after the tetanus stimulus (10-15mins), there is an increase in the amount of ACh packaged in vesicles, hence more ACh is released into the synaptic cleft with each stimulus
- The increased amount of ACh may displace enough NDMR from the ACh receptors (remember they are competitive antagonists) to overcome a partial block
- This results in the reappearance of twitches when there were none before and greater twitch strength
- This is the basis for using post-tetanic count to monitor the depth of paralysis when the train of four count is 0
Comparison of Agents
- Click here to download a Word doc with a table comparing muscle relaxants
- It includes a blank version
- You should memorise the key points, then fill the details into the blank version once per day until you have it memorised
- It's a grind, but it doesn't take that long to do
Factors Affecting Sensitivity to NDMRs
Factors That Potentiate NDMRs
- Non-depolarising neuromuscular blockers are competitive antagonists of the nicotinic ACh receptor at the neuromuscular junction
- Drugs can enhance the action of non-depolarising NMBs via either pre-synaptic or post-synaptic mechanism → prolong duration of action and ↓ dose required
Pre-Synaptic Mechanisms
- Drugs can reduce pre-synaptic release of ACh → enhance action of non-depol NMBs
- Block pre-synaptic ACh receptors → prevent positive feedback → ↓ ACh release
- eg volatile anaesthetics
- Reduce cAMP synthesis → ↓ ACh release
- eg frusemide
- Block pre-synaptic Ca2+ channels → ↓ ACh release
- eg volatile anaesthetics
- aminoglycosides, clindamycin, polymyxins (main mech of action)
- Ca+ channel blockers: probably minor clinical significance
- Magnesium
Post-Synaptic Mechanisms
- Drugs can interfere with ion flux through post-synaptic nicotinic receptors → enhance action of non-depolarising NMBs
- Direct blockade of post-synaptic ACh receptors
- Other non-depolarising neuromuscular blockers
- Volatile anaesthetics
- Aminoglycosides → ↓ nACh rec sensitivity to ACh (secondary mech of action)
- Quinidine
- Desensitisation block (binding to non-receptor sites)
- Volatiles
- Barbiturates
- Local anaesthetics: block fast Na+ channels ↓ Na+ conductance → ↓ membrane excitability
- Magnesium: inhibits post-junctional membrane potential generation → ↓ membrane excitability
- Lithium: ↓ membrane excitability
- Dantrolene: prevent release of Ca2+ from SR → ↓ mechanical response of muscle to stimulation → indirect potentiation of non-depolarising NMBs
- Anti-oestrogen drugs (e.g. tamoxifen) ?mechanism
Volatile agents
- Magnitude of potentiation depend on:
- Duration of inhalational anaesthesia
- Specific agent used. Des > sevo > iso > halo > N2O
- Concentration of agent used
- Proposed mechanisms
- Central effect on α motor neurones and interneurone synapses
- Direct ACh rec antagonism
- Augmentation of NDMRs affinity for binding site
Factors That Inhibit NDMRs
- Chronic anticonvulsant therapy →
- ↑ clearance of NDMRs
- ↑ binding of NDMRs to α 1-acid glycoprotein
- Upregulation of NMJ ACh receptors
- Hyperparathyroidism → ↑ Ca2+ →
- ↓ sensitivity to atracurium and pancuronium
- ?mechanism
Depolarising Muscle Relaxants
Mechanism of Action
- Structurally, suxamethonium is basically two acetylcholine molecules joined together
- It is an agonist at the NMJ nicotinic ACh receptor, just like acetylcholine
- The difference is that suxamethonium is not rapidly metabolised by acetylcholinesterase present in the NMJ - its effect is only terminated by removal from the NMJ by vascular uptake and metabolism by pseudocholinesterase in the plasma (also called plasma cholinesterase and butyrylcholinesterase)
- To understand how suxamethonium works, you need to understand
- Normal NMJ transmission (see section The Neuromuscular Junction → Normal NMJ Physiology)
- Voltage gated sodium channels (see section Local Anaesthetics → Pharmacodynamics → Voltage Gated Sodium Channels)
- Sequence of events
- Suxamethonium is administered iv/im and is delivered to the NMJ via the blood
- It binds to post-synaptic nic ACh receptors, activating the chain of events leading to excitation-contraction coupling , just like ACh would (causing initial fasciculations)
- Because suxamethonium is not rapidly broken down by AChE, it remains bound to the post-synaptic nic ACh receptor and keeps it activated, ie keeps the cation channel open → continuous influx of Na+ → keeps the cell membrane of the motor end plate depolarised
- This means that the surrounding Vg Na+ channels, which when initially activated cycled from the resting state → activated state → inactivated state, cannot cycle back to the resting state
- No further action potentials can be initiated from the motor end plate until the cell membrane repolarises past threshold to allow the Vg Na+ channels to cycle back to the resting state
Adverse Effects
Mneumonic
- Muscle pains
- Initial fasciculations from unco-ordinated, widespread NMJ ACh rec activation
- Apnoea, prolonged
- Small proportion of population don’ t have pseudocholinesterase
- Rise in pressures (intraocular, intracranial, intragastric)
- Relative contraindication in open eye injury, raised ICP
- K+ ↑
- ↑ 0.3-0.5mmol/L usually, due to sustained efflux of K+ through cation channel of activated nic ACh receptors
- Up to ↑ 3-5mmol/L in denervation injuries, burns, CVA, etc due to upregulation of abnormal, extrajunctional nic ACh receptors)
- Ectopics and other arrhythmias
- Due to stimulation of ACh rec in autonomic ganglia
- Temp rise (Malignant Hyperthermia)
- Pharmacogenetic disorder that is triggered by exposure to sux or volatiles
- Hypersensitivity
- Anaphylactic or anaphylactoid reactions
Muscle pains
- Initial fasciculations from unco-ordinated, widespread NMJ ACh rec activation
- Commonly causes moderate muscle soreness post-operatively
Prolonged Sux Apnoea
- May be due to
- pharmacogenetic disorder
- acquired pseudocholinesterase deficiency
- See section below Sux Apnoea
Rise in pressures
- Due to initial stimulation of muscle contraction → ↑ intraocular, intracranial and intragastric pressures
- Relative contraindication in open eye injury, raised ICP due to concern about extrusion of intraocular contents and coning
- The ↑ risk of regurgitation from ↑ intragastric pressure is offset by concomitant ↑ lower oesophageal tone
Hyperkalaemia
- ↑ K+ 0.3-0.5mmol/L usually
- Due to sustained efflux of K+ through cation channel of activated nic ACh receptors
- However, in some situations (denervation injuries, burns, CVA, spinal cord injury) the response may be exaggerated → ↑ K+ 3-5mmol/L → hyperkalaemic cardiovascular collapse
- Mechanism is related to upregulation of abnormal, extrajunctional nic ACh receptors → allow greater efflux of K+
Arrhythmias
- Ectopic beats are common with sux
- Both brady and tachy arrhythmias can be precipitated
- Due to stimulation of ACh recs in autonomic ganglia (sympathetic and parasympathetic)
Malignant Hyperthermia
- Pharmacogenetic disorder that may be triggered by exposure to suxamethonium or volatile agents
- Mechanism involves an abnormal ryanodine receptor that results in ↑ Ca2+ release from sarcoplasmic reticulum → sustained muscle contraction and hypermetabolism
- Mortality is high
- Treatment is with dantrolene
- Can be tested for with muscle biopsy, using caffeine-halothane contracture testing
Masseter Spasm
- Spasm of masseter muscle, particularly in kids, can impede intubation
- It is not clear whether this is a subtype of MH reaction or a separate entity
Hypersensitivity
- Can precipitate anaphylactic or anaphylactoid reactions
- Higher incidence than non-depolarising muscle relaxants
Phase II Block
- Suxamethonium usually causes a depolarising block, that is characterised by
- Initial fasciculations
- No fade or post-tetanic facilitation
- However, with repeated doses or an infusion, the characteristics of the block may change to become similar to a non-depolarising block - fade and post-tetanic facilitation are present
- The exact mechanism is not well understood, I believe, but one hypothesis is that there is rapid tachyphylaxis, some mechanism of reduced sensitivity to the effects of suxamethonium
- The way I conceptualise it is that the ACh receptors become resistant to being activated by sux (and hence also resistant to activation by ACh), and some of them effectively become "inactive" and only a proportion of the total receptors can still be activated by binding by an agonist
- Once enough of the receptors became "inactive", there would no longer be enough activated receptors to keep the motor end plate depolarised and you would lose the depolarising block
- However, now you have a situation that is similar to when there is a non-depolarising block where a proportion of the receptors are made "inactive" by binding by an antagonist, so it makes sense that the characteristics of the block would become like a non-depolarising block
- I just pulled that rationalisation out of my ass, so I don't know how true it is, but for exam purposes, don't worry about it, if you are being asked about this in a viva, I'm sure you are already in medal contention
Sux Apnoea
- Patients with reduced pseudocholinesterase activity may exhibit prolonged paralysis after suxamethonium administration
- May be due to
- Genetic variability (pharmacogenetic disorders)
- Acquired deficiency
Pharmacogenetic Disorders
- There are 4 alleles (alternative variations of a gene) identified on Chromosome 3 that affect pseudocholinesterase activity
- Normal plasmacholinesterase activity
- Usual (Eu) aka normal
- Reduced plasmacholinesterase activity
- Atypical (Ea) aka "dibucaine-resistant"
- Silent (Es)
- Fluoride-resistant (Ef)
- 96% of population are homozygous for the normal gene, Eu:Eu
- Almost 4% of population are heterozygous with one normal and one abnormal gene, that confers mildly prolonged duration of block (up to 10 mins)
- A very small proportion of population have two abnormal genes, resulting in prolonged block (several hours)
| Genotype | Incidence | Duration of block | Dibucaine number |
| Eu:Eu | 96% | normal | 80 |
| Eu:Ea | 1:25 | + | 60 |
| Eu:Es | 1:90 | + | 80 |
| Eu:Ef | 1:200 | + | 75 |
| Ea:Ea | 1:2800 | ++++ | 20 |
| Ea:Ef | 1:20 000 | ++ | 50 |
| Es:Ea | 1:29 000 | ++++ | 20 |
| Es:Es | 1:100 000 | ++++ | − |
| Ef:Es | 1:150 000 | ++ | 60 |
| Ef:Ef | 1:154 000 | ++ | 70 |
Dibucaine Number
- Dibucaine is an amide local anaesthetic that also has the property of inhibiting normal pseudocholinesterase (reduces activity by 80%)
- Dibucaine is less effective at inhibiting abnormal pseudocholinesterase (reduces activity by 20-80%, depending on the gene combination)
- The dibucaine number refers to the % inhibition of pseudocholinesterase activity
Acquired Deficiency
- Pregnancy
- Liver disease
- Renal failure
- Cardiac failure
- thyrotoxicosis
- Cancer
- Drugs – either directly or by acting as substrate or inhibitor to AChE
- Metoclopramide
- Ketamine
- Oral contraceptive pill
- Lithium, lidocaine
- Ester local anaesthetics
- Cytotoxic agents
- Edrophonium, neostigmine
- Trimetaphan
Reversal Agents
Anti-Cholinesterase/Anti-Muscarinic Combo
Anti-cholinesterase/Anti-muscarinic Combo
- Non-depolarising block can be "reversed" using an anti-cholinesterase drug such as neostigmine
- By inhibiting acetylcholinesterase at the NMJ from breaking down the ACh that is released into the synaptic cleft, the concentration of ACh that reaches the post-synaptic ACh receptors is greatly increased
- NDMRs are competitive antagonists to ACh, so by increasing the ACh concentration, this shifts the balance of binding to the nic ACh receptor in favour of ACh
- If the balance is shifted enough, then enough nic ACh receptors can be activated to depolarise the motor end plate to threshold and re-establish signal transmission across the NMJ
Why do we need to add an anti-muscarinic?
- The anti-cholinesterase drugs not only affect the NMJ, but also affect the autonomic system synapses that use ACh as the neurotransmitter - mainly the post-ganglionic parasympathetic fibres that release ACh that acts on muscarinic ACh receptors
- If an anti-muscarinic drug were not given in combination with the anti-cholinesterase, it would cause unopposed parasympathetic stimulation resulting in bradycardia, ↑ secretions, miosis, ↑ peristalsis, etc
Neostigmine/Atropine or Neostigmine /Glycopyrrolate?
- Neo/atropine used to be the common combo because glyco was expensive, but neo/glyco has now become the routine choice because of 2 advantages
- Onset and duration of action
- neo and glyco have similar times to onset and durations of action, hence "cancel out" each other better
- atropine has a faster onset and shorter duration than neo, potentially resulting in early tachycardia then late bradycardia
- Central anticholinergic syndrome
- glyco is a quaternary amine and cannot cross the blood-brain barrier, while atropine is a tertiary amine and can cross the BBB and potentially cause central anticholinergic syndrome, particularly in elderly patients
Why can't a deep block be reversed?
- To reliably reverse a block, a TOFC of at least 2 - preferably 4 - is advisable before attempting reversal
- This is because of the ceiling effect of neostigmine
- There is a finite amount of ACh at the NMJ
- Once all the AChE has been inhibited, further increasing the dose of neostigmine will not result in higher ACh concentration
- Hence a deep level of block cannot be antagonised using this method. Contrast this with sugammadex, which can be used to reverse a deep block
Anti-Cholinesterase Drugs
- Click here to download a Word doc with a table comparing anticholinesterases
- It includes a blank version
- You should memorise the key points, then fill the details into the blank version once per day until you have it memorised
- It's a grind, but it doesn't take that long to do
Anti-Cholinergic Drugs
- Click here to download a Word doc with a table comparing anticholinergics
- It includes a blank version
- You should memorise the key points, then fill the details into the blank version once per day until you have it memorised
- It's a grind, but it doesn't take that long to do