Definitions
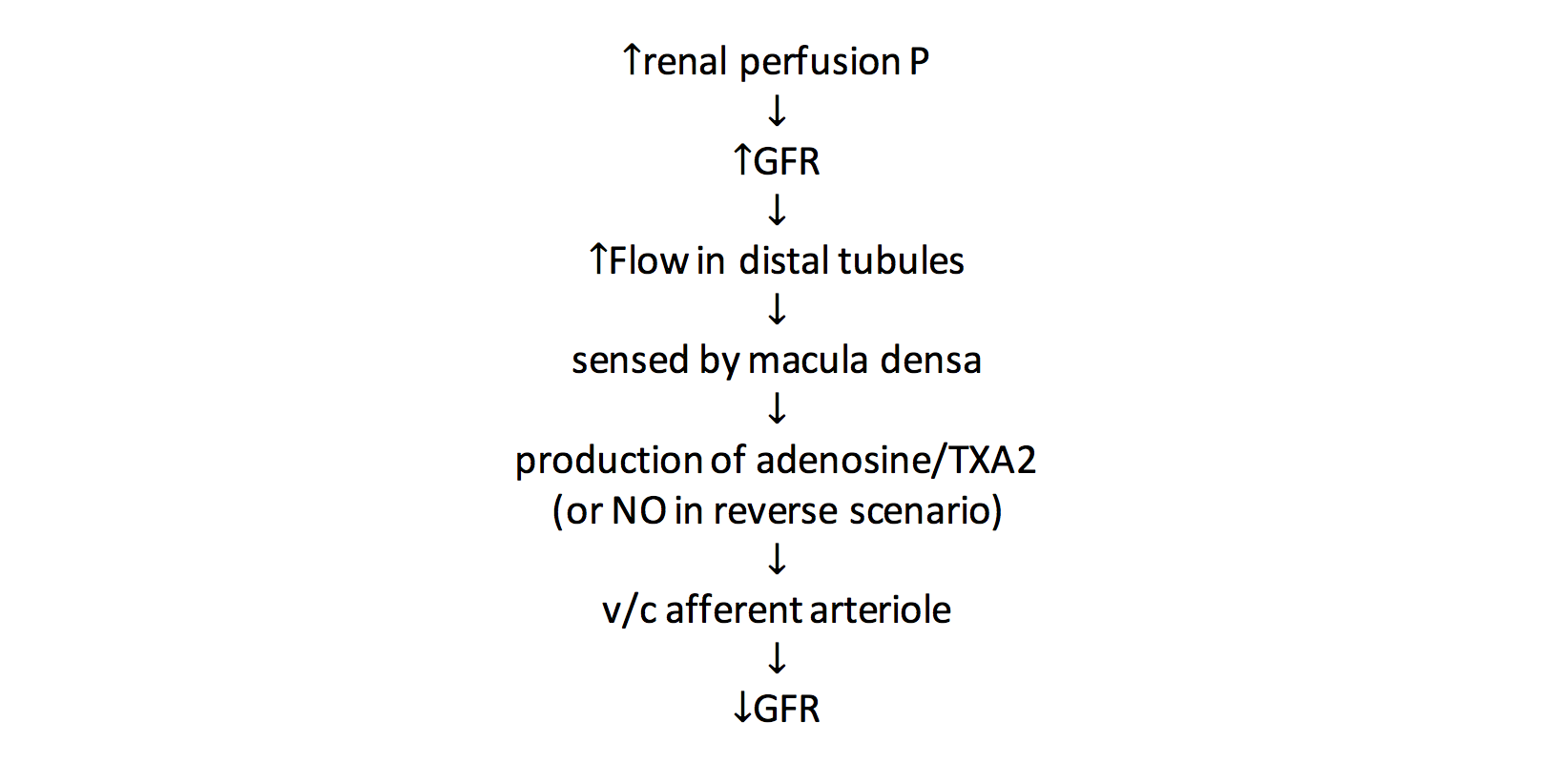
Tubuloglomerular Feedback
- Feedback mechanism that aims to maintain constant GFR and rate of water and solute load delivery to the distal tubules, in the face of changing renal perfusion
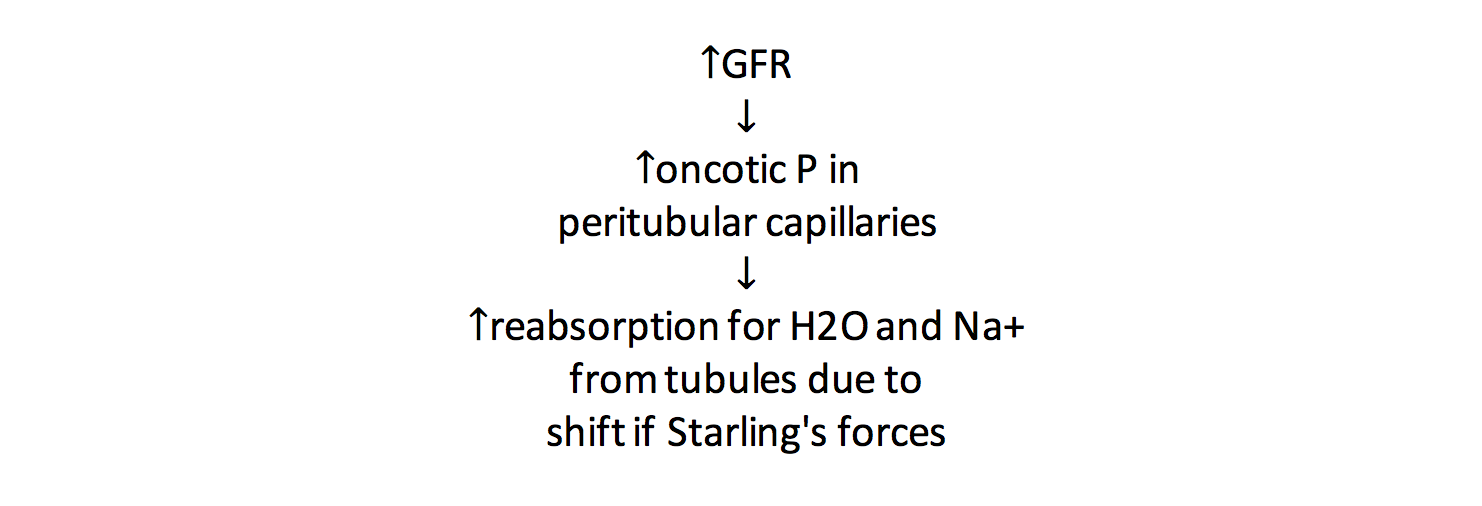
Glomerulotubular Balance
- Mechanism that maintains constant fraction of fluid and solute reabsorption from the tubules, despite changes in GFR
Functions of the Kidney
Overview
- Water and electrolyte homeostasis
- glomerular filtration (125ml/min = 180L/day)
- tubular reabsorption (PCT reabsorbs 60% of water and Na+)
- tubular secretion
- Excretion of waste products
- urea (protein)
- creatinine (muscle)
- uric acid (nucleic acids)
- bilirubin (Hb)
- Hormone production
- Gluconeogenesis
- Acid-base balance
- Excretion of drugs and chemicals
Water Balance
| Input | Output | ||
|---|---|---|---|
| Drink | 1200ml | Insensible | 900ml |
| Food | 1000ml | Sweat | 50ml |
| Metabolic | 350ml | Faeces | 100ml |
| Urine | 1500ml | ||
| Total | 2550ml | Total | 2550ml |
Obligatory urine loss
- 700mmol waste products/day
- max urine osmolality 1400mosmoles/kg
- Hence minimum water loss 500ml/day
Free water
- non-osmotically obligated water
- the water in excess of that required to produce a solution of the same osmolality as plasma
Electrolyte Requirements
| Na+ | 100-150mmol/day |
| K+ | 70-100mmol/day |
| Cl- | 150mmol/day |
| Urea | 400mmol/day |
Endocrine Functions
- Production of hormones in the kidney
- 1,25 dihydrocholecalciferol
- Calcitriol, active form of Vit D
- Produced in PCT
- EPO
- Produced by endothelial cells of peritubular capillaries
- in response to renal hypoxia
- Prostaglandins
- Release of enzymes that initiate hormone production extrinsically
- Renin → Ang II → aldosterone
- Kallikrein → bradykinin
- Hormones that act on the kidney
- ADH
- aldosterone
- calcitiriol
- PTH
- ANP
- Produced in right atrium in response to ↑ stretch
- Relax glomerular mesangial cells → ↑ GFR
- v/d aff and v/c eff arterioles → ↑ GFR
- ↓ ADH release, ↓ aldosterone
- Inhibit Ang II
- v/c effect
Renal Blood Flow
Normal Values
- 1200ml/min
- 25% of CO (x10 its metabolic requirements)
Measurement
- p-aminohippuric acid (PAH) is filtered by glomerulus and secreted by tubules
- Has a high extraction ratio (ER) = 0.9
- Effective renal plasma flow (ERPF) = clearance of PAH (ignores the fact that ER not quite 1)
- ERPF = UPAH.V/PPAH
- UPAH - urinary concentration of PAH
- V - volume of urine
- PPAH - plasma concentration of PAH
-
RBF = ERPF/ER . 1/(1 - hct)
- hct - haematocrit
Control of RBF
- Autoregulation
- myogenic mechanism (70-170mmHg)
- tubuloglomerular feedback
- Sympathetic innervation
- RAAS system
- Atrial natriuretic peptide
- Eicosanoids
- Noradrenaline → v/c internolar arteries and afferent arterioles
- Dopamine (made in kidney) → renal v/d and natriuresis
- Ang II → v/c efferent > afferent arterioles
Autoregulation
- Myogenic mechanism (70-170mmHg)
- Tubuloglomerular feedback
Tubuloglomerular Feedback
- Feedback mechanism that aims to maintain constant GFR and rate of water and solute load delivery to the distal tubules, in the face of changing renal perfusion
- Macula densa
- Sensor of fluid and NaCl flow rate in distal tubule
- Produces locally vasoactive agents in response to changes in flow
- adenosine (v/c)
- TXA2 (v/c)
- NO (v/d)
Glomerulotubular Balance
- Mechanism that maintains constant fraction of fluid and solute reabsorption from the tubules, despite changes in GFR
- Don't get tubuloglomerular feedback and glomerulotubular balance mixed up!
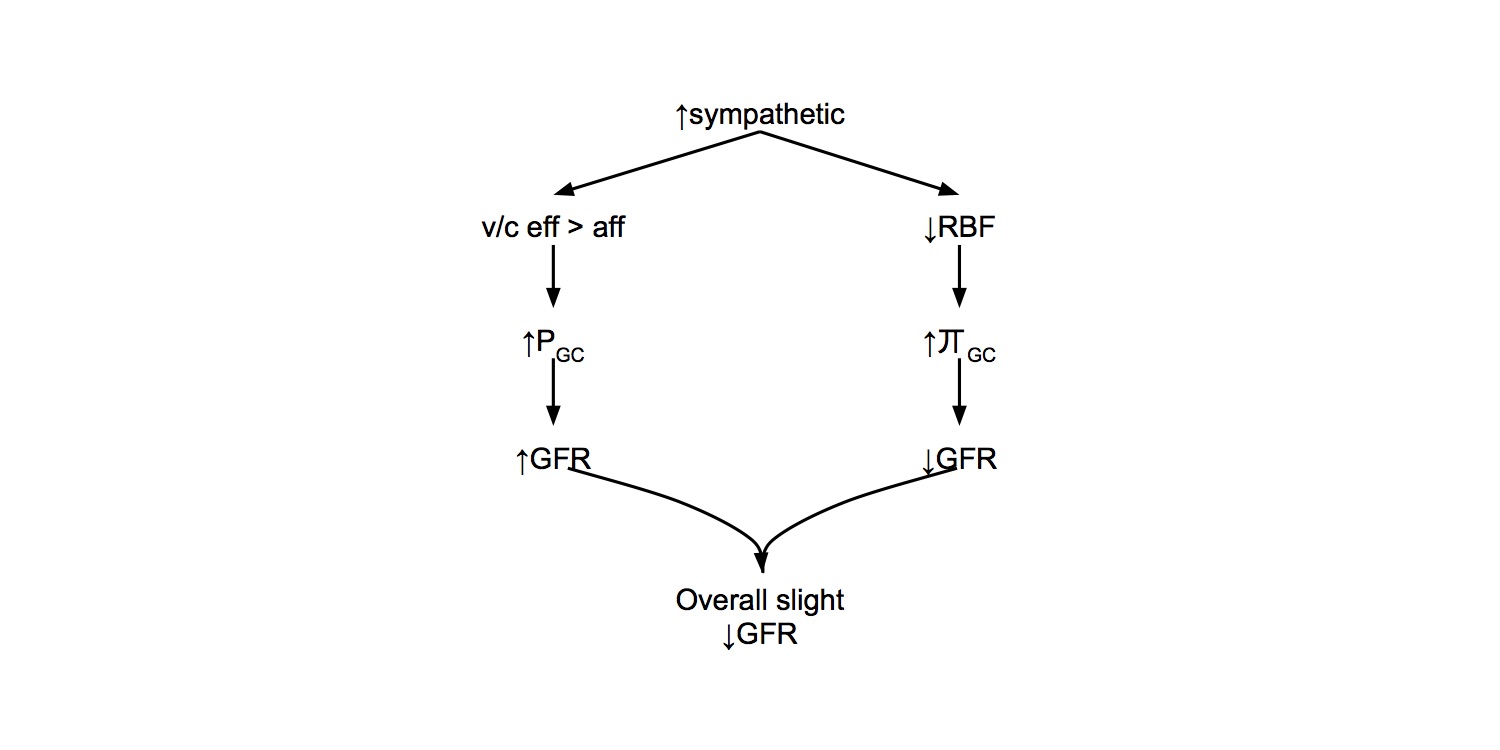
Sympathetic Innervation
- Low thoracic to high lumbar sympathetic outflow
- Sympathetic stimulation results in ↓ RBF, but only a slight reduction in GFR
Renin
- Renin secreted by juxtaglomerular cells
Control of renin secretion
Increased
- ↑ sympathetic
- ↑ circulating catecholamines
- ↓ aff arteriole P
- ↓ flow past macula densa
Decreased
- Ang II
- ADH
Angiotensin
Production
Angiotensin II actions
- Adrenal cx → ↑ aldosterone secretion
- ↑ Facilitation of NA release from sympathetic nerves
- Contraction of mesangial cells → ↓ filtration coeff → ↓ GFR
- Thirst (OVLT, SFO)
- ↑ Secretion of ADH and ACTH (area postrema)
End results:
- Renal salt and water retention
- ↑ SVR
- ↑ CO
- ↑ Arterial pressure
Aldosterone
- Steroid hormone produced by zona glomerulosa of adrenal cortex
- Release stimulated by
- Ang II
- ↑ plasma [K+]
- ACTH
- Actions
- Stimulates Na+ reabsorption and K+ secretion by principal cells of the cortical collecting ducts
- Stimulates H+ secretion by type A intercalated cells
Anti-Diuretic Hormone
- Synthesised in hypothalamus
- Secreted by post pituitary
- ↑ water permeability of CD luminal membrane → ↑ water reabsorption
- Acts via cAMP → insert aquaporin 2 channel
- At high concs acts as vasoconstrictor
- ↓ RBF
- ↓ GFR
- Secretion stimulated by
- ↑ osmolality > 1% change (osmoreceptor in hypothalamus OVLT)
- hypovolaemia > 5-10% change (low P barorec)
- hypotension (high P barorec)
- Ang II
- Pain, stress, emotion
- nausea and vomiting
- carbamazepine
- (alcohol → ↓ secretion)
Atrial Natriuretic Peptide
- Produced in right atrium in response to ↑ stretch
- Relax glomerular mesangial cells → ↑ GFR
- v/d aff and v/c eff arterioles → ↑ GFR
- ↓ ADH release, ↓ aldosterone
- Inhibit Ang II
- v/c effect
Eicosanoids
- PGI2 and PGE2 are locally active vasodilators produced by kidney in clinical states associated with high concs of circulating vasoconstrictors
- Inhibition of COX in these states may ↓ RBF and impair renal function
Glomerular Filtration
Normal Values
- 125ml/hr
- 180L/day
- NB only 500ml-1L urine produced per day, meaning that > 99.4% of filtered water is normally reabsorbed by the kidneys
- This also means that if there is tubular dys function and impaired reabsorption of water, there is huge potential for excessive water loss (polyuric renal failure)
Balance of Starling's Forces
- Net fluid flux = k. [(PC - PBC) - σ (π C - π BC)]
- k - filtration coefficient
- incorporates SA and hydraulic conductivity
- high in glomerulus due to many fenestrations
- σ - reflection coefficient (= 1)
- PC - capillary hydrostatic pressure
- PBC - Bowmans capsule hydrostatic pressure
- π C - capillary oncotic pressure
- π BC - Bowmans capsule oncotic pressure
| Capillary | afferent end | efferent end |
| PC | 60 | 58 |
| PBC | 15 | 15 |
| π C | 21 | 33 |
| π BC | 0 | 0 |
| net filtration P | 24 | 10 |
Glomerular Capillary Hydrostatic Pressure
- Balance between relative resistances of afferent and efferent arterioles
- ↑ with ↑ sys P minimised by autoregulation (70-170mmg)
Glomerular Capillary Oncotic Pressure
- ↑ sympathetic → ↓ RBF → ↑ π C due to filtration → ↓ net filtration P → ↓ GFR
Glomerular filtrate
- < 7,000 Da → freely filtered
- > 7,000 Da → ↓ ing filtration
- > 70,000 Da → no filtration
- Surface of glomerular filtration barrier has negative charge
Filtration Fraction
- GFR/RPF = 125/600 = 20%
Control of Urine Output
Simplified Schematic
- This simple schematic shows how the main homeostatic mechanisms fit in together
- It should be fairly easy to remember in this format, but ideally in an exam answer it should be fleshed out with more detail (see Full Schematic)
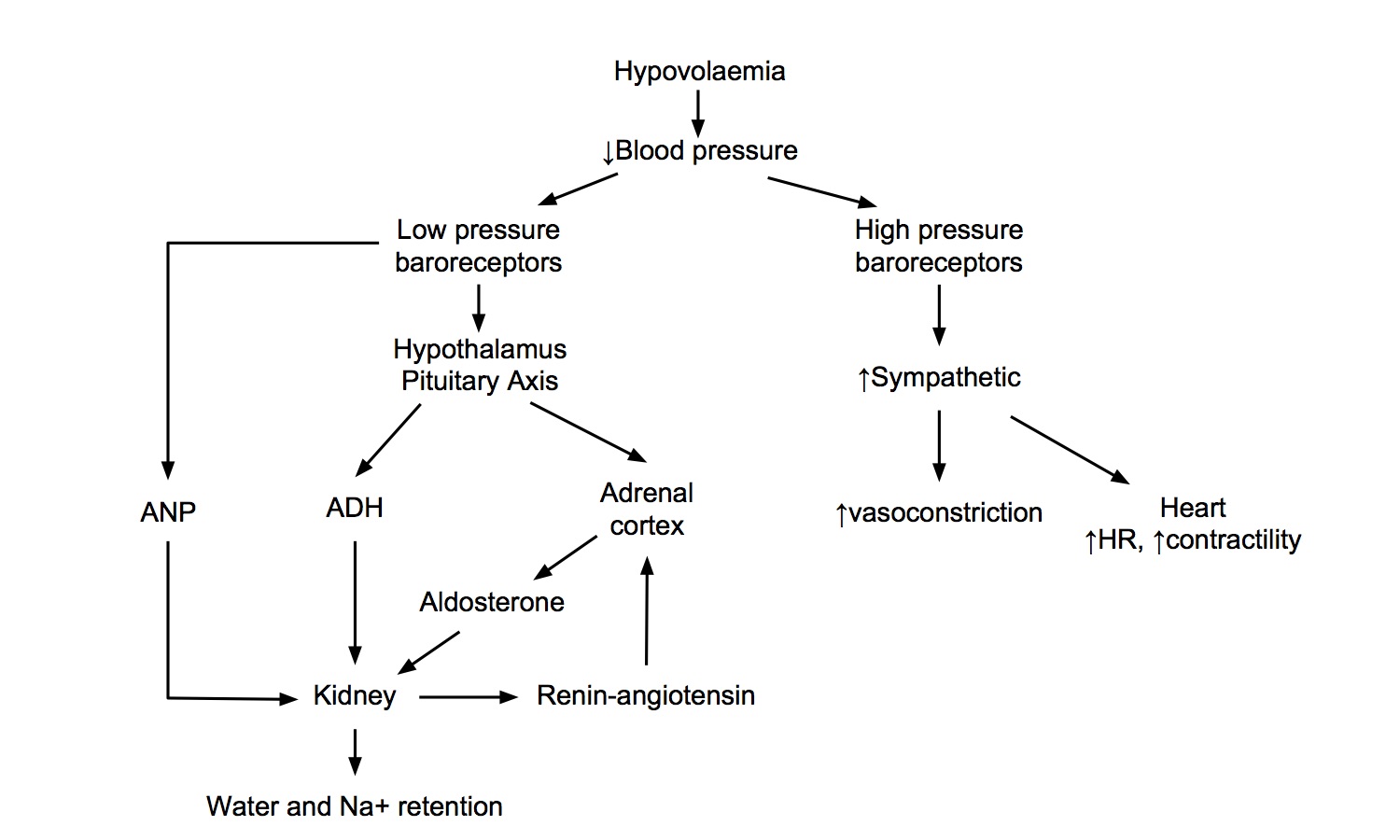
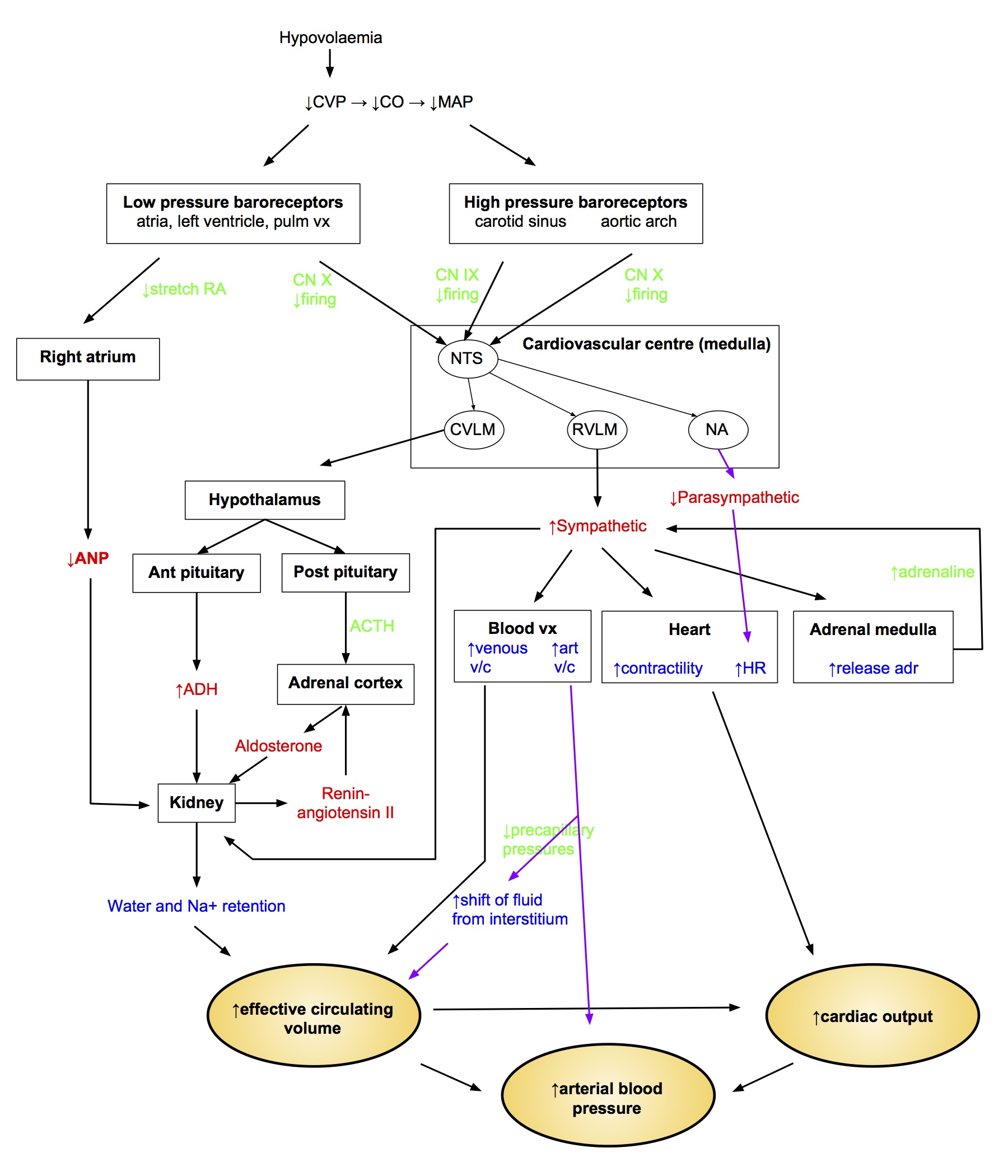
Full Schematic
- This crazy busy schematic shows how all of the homeostatic mechanisms fit in together
- There's no way you would have time to reproduce this in full during the exam, but I think it is useful to try and get your head around how everything integrates together