Definitions
Thermoregulation
- Homeostatic process that aims to maintain a constant core temperature
Core Temperature
- The temperature of the main internal organs
Hypothermia
- An abnormally low core body temperature, below the physiological normal limit
- Mild - > 32C to 35C
- Moderate - 28C to 32C
- Severe - < 28C
Hyperthermia
- An elevated core body temperature, above the physiological normal limit
Interthreshold Range
- The range of core temperatures over which no autonomic thermoregulatory responses occur
Thermoneutral Zone
- The range of environmental temperatures over which metabolic heat production (and hence O2 consumption) is minimal and core body temperature can be maintained by changes in vasomotor activity to skin blood vessels alone
Radiation
- Transfer of heat by infrared electromagnetic radiation from one object to another at a different temperature with which it is not in contact
Convection
- The transfer of heat by the circulation or movement of the heated parts of a liquid or gas
Conduction
- Heat exchange between objects at different temperatures that are in direct contact with one another
Evaporative Loss
- The loss of the latent heat of vaporization when a substance (water) changes phase from liquid to gas
Latent Heat of Vaporization
- The heat absorbed when a substance changes phase from liquid to gas
Balance of Heat Production/Loss
Heat Production
- All energy used by the body is ultimately converted to heat energy
- Main sources of heat production are
- Basic metabolic processes (under endocrine control)
- Food intake (specific dynamic action)
- Muscular activity
- Heat production varies with catecholamines, thyroid hormone
Heat Loss
| Mechanism | Contribution |
|---|---|
| Radiation | 40-50% |
| Convection and conduction | 15% |
| Evaporation from skin | 30% |
| Evaporation from resp tract | 5% |
| Urination and defaecation | 1% |
Effects of Hypo/Hyperthermia
Effects of Hypothermia
Thermoregulatory Responses
- Cutaneous vasoconstriction
- Shivering
- Non-shivering thermogenesis (in neonates)
- Behavioural changes
Pathological Responses
- CVS
- ↓HR – slowing of discharge from SA node
- Paradoxical vasodilation – from direct cold-induced paralysis of peripheral blood vessels – followed by alternating vasoconstriction and vasodilation (“hunting reaction”) that serves to prevent frostbite
- CNS
- < 34C → mental confusion
- < 32C → loss of consciousness
- M/skel
- 35C → muscle weakness, ↓ shivering
- Haem
- Coagulopathy
Effects of Hyperthermia
Thermoregulatory Responses
- Cutaneous vasodilation
- Sweating
- Behavioural changes
Pathological Responses
- CVS
- ↑HR, ↑CO
- BP remains stable due to vasodilation
- CNS
- Irritability → heat stroke
- > 42C → loss of consciousness
- M/skel
- Fluid and electrolyte loss → muscle cramps
Thermoregulatory Homeostatic System
Schematic
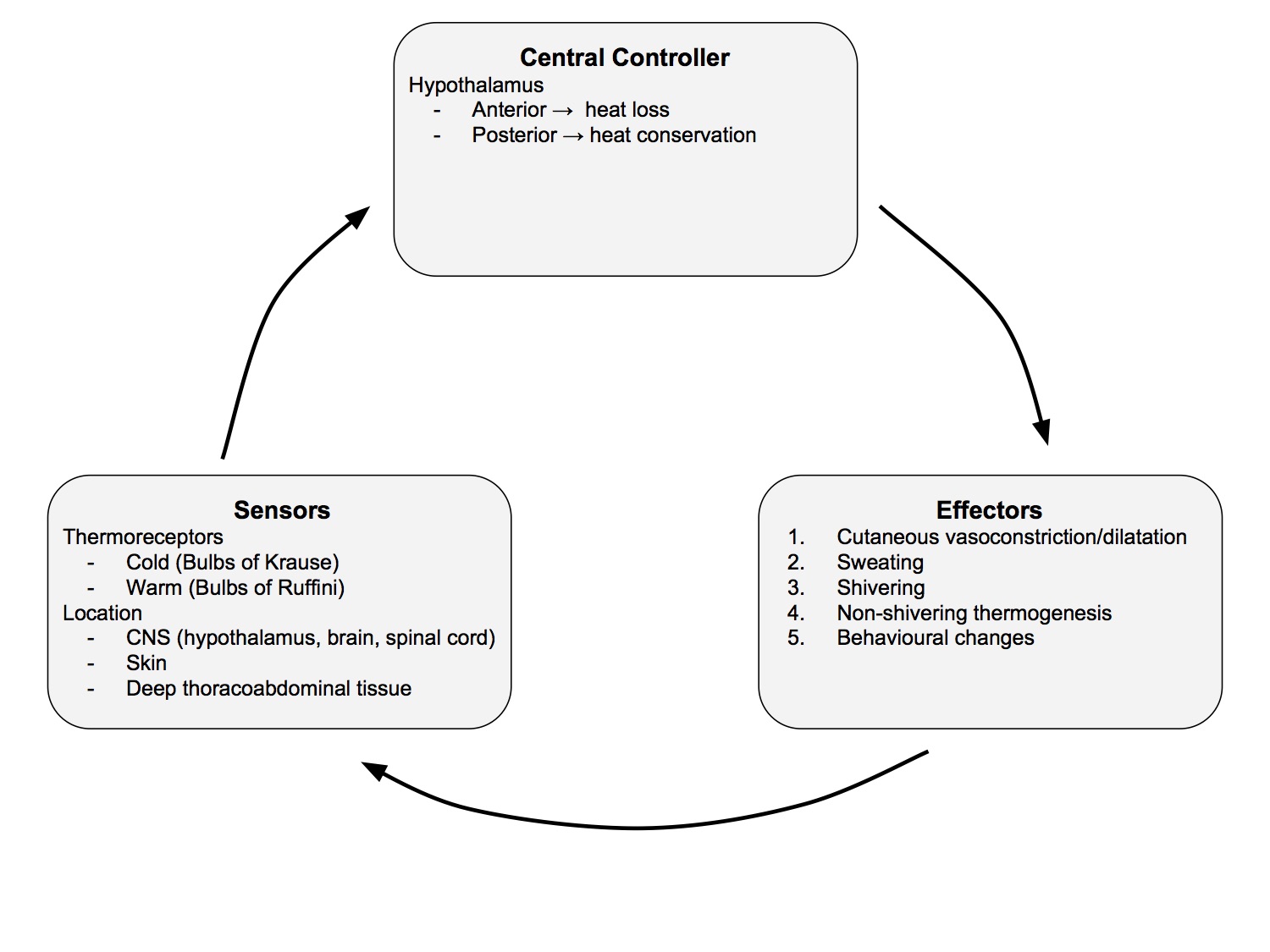
- Over a wide range of ambient temperatures, core temperature is kept constant, within 0.4C of set point 37C
Sensors
- Skin thermoreceptors (for hot and cold) monitor environmental temperature
- cold receptors
- bulbs of Krause in dermis
- transmit impulses to hypothalamus via Aδ fibres
- Exhibit static (regular and periodic) discharges at constant temp and increase below 24-25C
- warm receptors
- bulbs of Ruffini
- Exhibit static discharges between 30 - 40C, maximal discharge rate at 44C, cease at 46C
- Impulses transmitted by C fibres (hence can't distinguish intense heat from sharp pain)
- Other thermoreceptors located in brain, spinal cord, deep thoracic and abdominal tissues
- Traverse mainly spinothalamic tracts (but also other pathways) to hypothalamus
- Hypothalamic thermoreceptors monitor core temperature
- Contributions to thermal input to hypothalamus:
| hypothalamus | 20% |
| other parts of brain | 20% |
| spinal cord | 20% |
| deep thoracic and abdominal tissues | 20% |
| skin | 20% |
Central Controller
- Hypothalamus
- Receives neural input from all thermoreceptors
- Responses are stimulated when core temperature moves outside the limits of the interthreshold range
- Stimulation of anterior hypothalamus (sensitive to local warming of blood) → initiate mechanisms for heat loss
- sweating
- vasodilatation
- Stimulation of the posterior hypothalamus → initiate mechanisms for heat conservation and production
- shivering
- vasoconstriction
Interthreshold Range
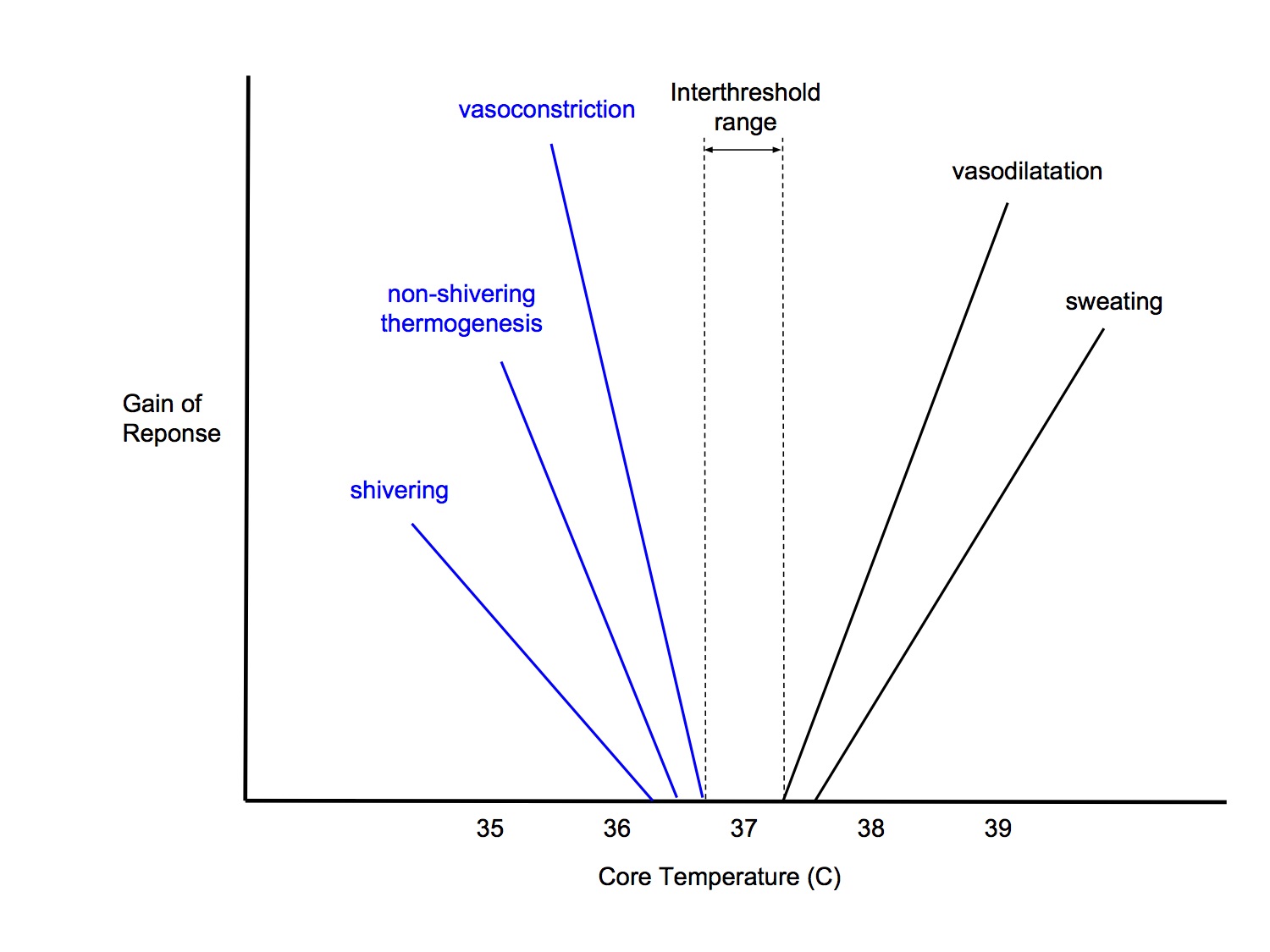
- The range of core temperatures over which no autonomic thermoregulatory responses occur
- Approx 37C +/- 0.2C in non-anaesthetised state
- Above the interthreshold range, sweating and vasodilatation occurs
- Below the interthreshold range, vasoconstriction, non-shivering thermogenesis and shivering occur
- The posterior hypothalamus establishes the set point around which body temperature is maintained
- This set point is determined by the ration of sodium to calcium ions in the posterior hypothalamus
- Threshold temps are influenced by
- circadian rhythm
- food intake
- thyroid function
- drugs
- thermal adaptation to warm or cold ambient temperatures
- Thresholds are 0.3 - 0.5C higher in women
- Slope of the intensity of response to difference between thermal input and threshold temperature is called the 'gain' of the response
Effectors
- Cutaneous vasoconstriction/dilatation
- Sweating → skin heat loss (sympathetic cholinergic)
- Shivering - controlled by a centre in hypothalamus
- Non-shivering thermogenesis
- heat production by effects on metabolic rate
- importance of brown fat in infants
- not significant in adults
- Behavioural responses
- level of activity
- posture
- amount of clothing
- absent in anaesthetised patient
- Other
- Thyroid hormone secretion (TRH secreted by hypothalamus)
- Piloerection (not important in humans)
Role of Skin
- Skin plays an important role in heat regulation
- large surface area in contact with environment
- has temperature sensors
- has effector mechanisms
- skin vasoactivity change
- sweating → evaporative loss
- When skin temp exceeds 30C → ↓ sympathetic activity to skin → vasodilation → ↓ vasc resistance → ↑ cardiac output and massive ↑ skin blood flow accomodated in dilated arteriovenous shunts and venous plexuses.
- Cutaneous blood flow can increase 30-fold in heat stress and decrease 10-fold in cold stress
- Sweating
- Max rate of sweating is 3L/hr, but cannot be sustained
- Max amount of sweat is 12L/day
Shivering Thermogenesis
- Involuntary contraction of muscles, controlled by hypothalamus
- Can ↑ metabolic rate by 100%
- Rapid tremors up to 250Hz of unsynchronized muscle activity
- Slow synchronous waves (4 - 8 cycles/min) are superimposed on fast tremors
- Cyclical muscle rigors 10-20Hz appear as shivering becomes more intense
Non-shivering Thermogenesis
- Increases metabolic heat production without mechanical work
- Activated by β 3 sympathetic activity which uncouples oxidative phosphorylation in brown fat and skeletal muscle
- In neonate, brown fat is found in interscapular region, perinephric fat and around intra-abdominal organs
- Brown fat is high vascular with abundant mitochondria and richly innervated by adrenergic fibres
- In neonate, non-shivering thermogenesis can increase metabolic rate two-fold
Thermoneutral Zone
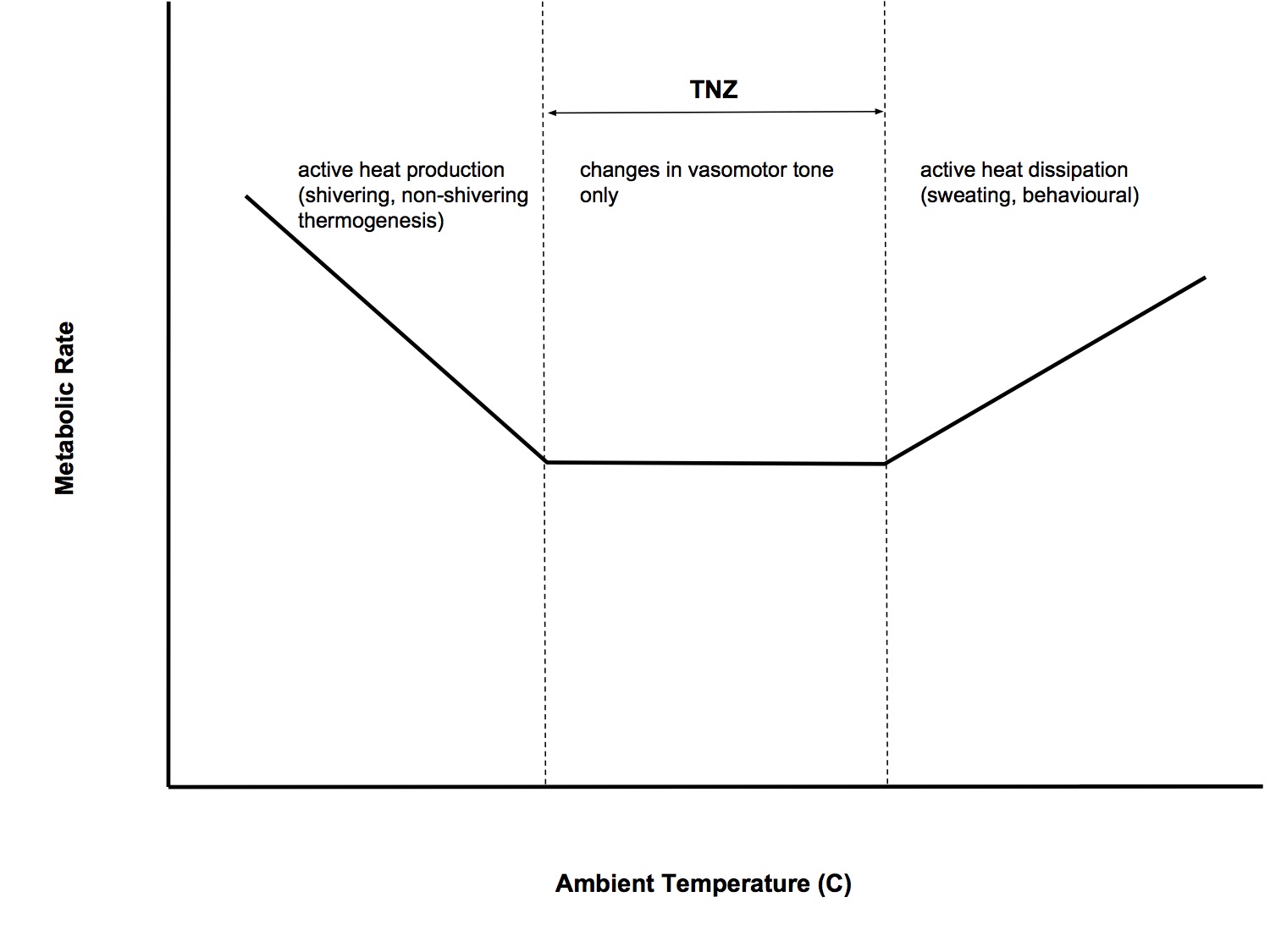
- The range of environmental temperatures over which metabolic heat production (and hence O2 consumption) is minimal and core body temperature can be maintained by changes in vasomotor activity to skin blood vessels alone
- Skin temperature is maintained at about 33C
- Below the critical temperature (27C), metabolic rate ↑ linearly as temp ↓
- Above critical temp, metab rate remains constant until an upper limit is reached, then it rises again
- TNZ in 70kg naked man is 27-31C
- Clothed adult TNZ 22 - 28C
- Clothed neonate TNZ 32 - 34C
Effects of Anaesthesia
Effects of General Anaesthesia
- Increases the interthreshold range from 0.2C to 4C
- ↓ threshold to cold by 2.5C
- ↑ threshold to warmth by 1.3C
- Within this expanded interthreshold range, active thermoregulatory responses are absent and body temperature changes passively, depending on balance of heat production and heat loss, ie poikilothermic (internal body temperature varies in parallel to ambient temperature)
- Behavioural responses are irrelevant in the unconscious, anaesthetised patient
- The only thermoregulatory response available to anaesthetised, paralysed and hypothermic patients are
- vasoconstriction
- non-shivering thermogenesis
- Gain and maximum intensity of some responses remain normal whereas other responses are reduced by general anaesthesia
- Dose-dependent response
- Propofol and alfentanil produce linear reduction in threshold for vasoconstriction and shivering vs dose
- Volatile agents produce a non- linear reduction, resulting in greater inhibition of vasoconstriction and shivering than propofol at commonly used anaesthetic doses
- Non-shivering thermogenesis is absent in anaesthetised adults and infants
- This is not significant for adults, but is important in infants
- Exposed to cold stress from OT environment
- Cold ambient temp
- Exposed body parts, open cavities
- Cold iv fluids
Development of Hypothermia During General Anaesthesia
- General anaesthesia typically results in mild hypothermia of 1-3C
- Hypothermia results from a combination of
- anaesthetic-impaired thermoregulatory responses
- exposure to cold OR environment
- Heat loss
- Radiation - major type of heat loss in most surgical patients, particularly if open, exposed abdomen
- Convective - 2nd most important mechanism. Minimised by covering with surgical drapes
- Conductive - minimal, as foam pad covering operating table is a good insulator
- Evaporative - insensible water loss is small in adults but is more significant in infants. Sweating is rare under anaesthesia
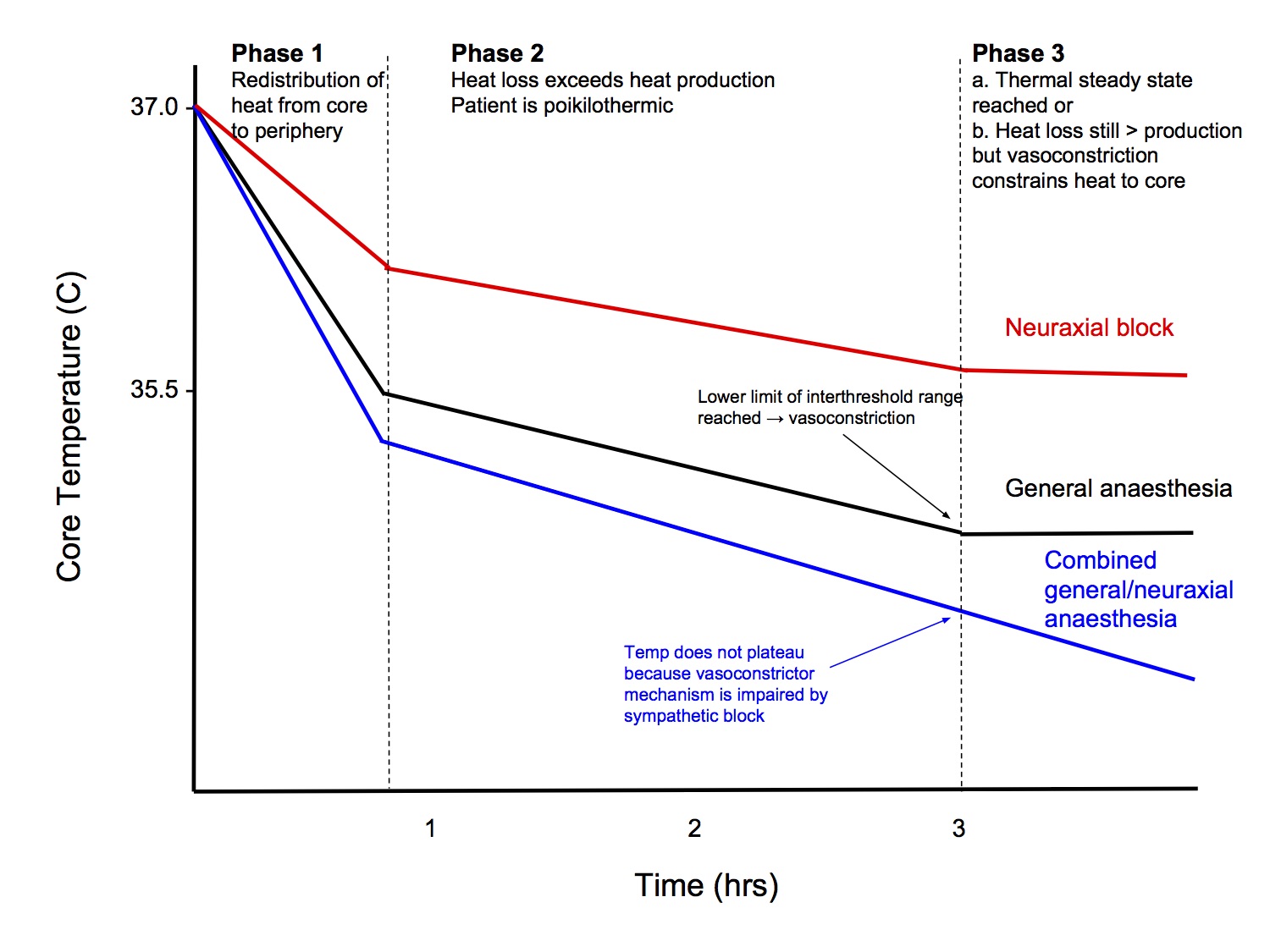
Pattern of Intraoperative Hypothermia
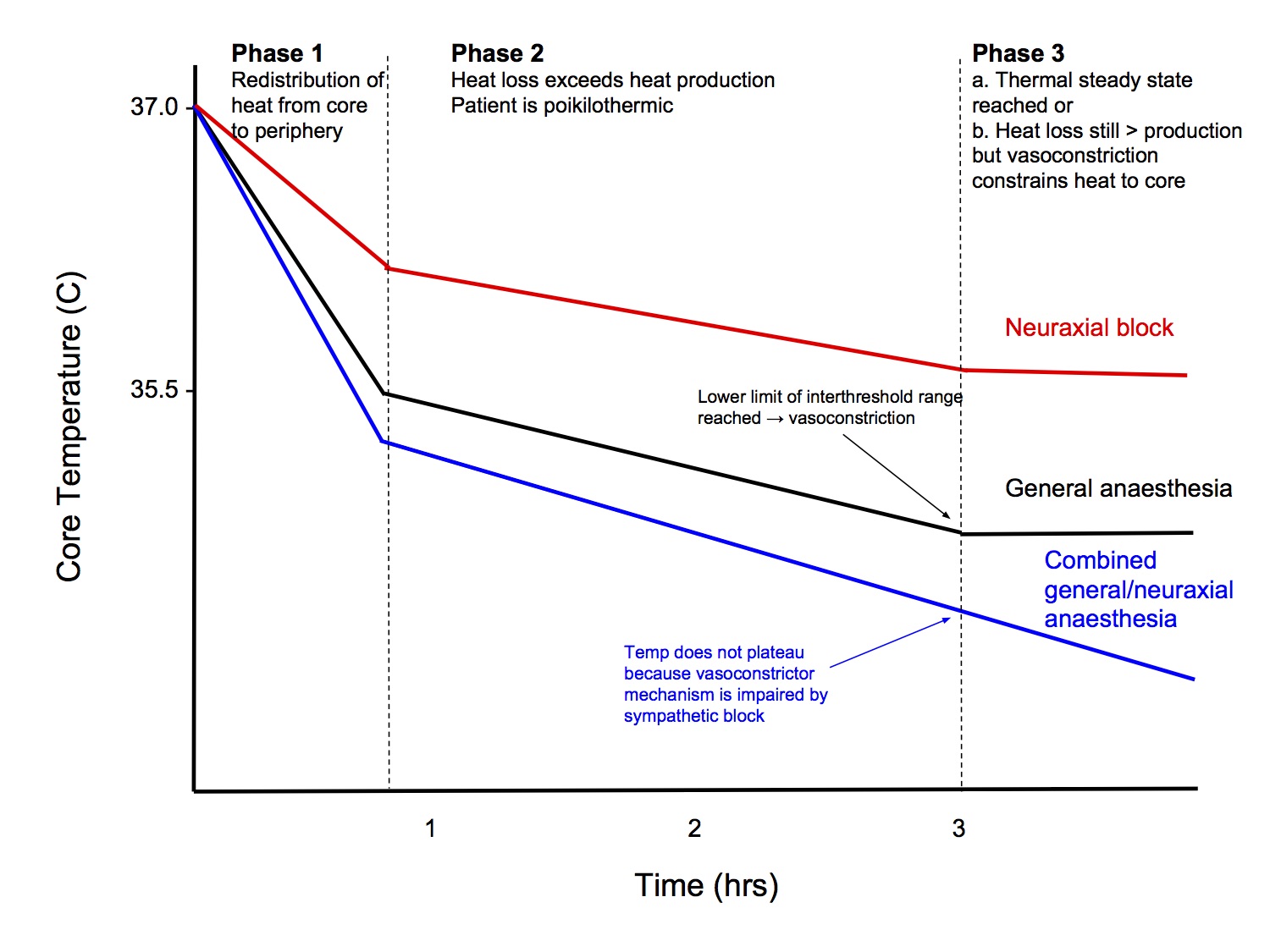
Phase 1 (1hr, ↓ 0.5-1.5C)
- Initial, rapid reduction in core temperature
- Mainly due to redistribution of heat from core to periphery
- Anaesthetic-induced vasodilation allows core heat to flow peripherally
- Extent to which redistribution reduces core temperature depends on the core-to-peripheral temperature gradient at the time of induction
- Minor contribution from
- Inhibition of thermoregulatory cutaneous vasoconstriction → ↑ heat loss
- ↓ metabolic rate 20 - 30% → ↓ heat production
Phase 2 (2 - 4hrs)
- Slower, linear reduction in core temperature
- Results simply from heat loss exceeding metabolic heat production (patient is poikilothermic within the expanded interthreshold range)
Phase 3
- Core temperature plateaus and stabilises
- May represent
- a thermal steady state (heat production = heat loss) or
- Core temp drops below lower limit of interthreshold range → trigger thermoregulatory vasoconstriction → constrains metabolic heat to core thermal compartment, prevents further ↓ core temp. Periph temp continues to decline, ie not a thermal steady state, heat loss remains > heat production
Effects of Neuraxial Anaesthesia
Neuraxial Anaesthesia
- Epidural and spinal anaesthesia both produce similar inhibition of autonomic thermoregulatory responses
Effects on Sensors and Central Processing by Hypothalamus
- Decrease threshold to trigger vasoconstriction and shivering by 0.6C
- Reduction in threshold is proportional to the number of spinal segments blocked
- Effects are result of local actions on spinal cord and not due to systemic recirculation of local anaesthetic (iv administration of lignocaine has no thermoregulatory effect)
- Mechanism
- Thermal input from lower limbs is dominated by tonic signals from cold thermoreceptors
- Regional anaesthesia blocks these cold signals
- Brain interprets the decrease input as relative leg warming → ↓ threshold that triggers vasoconstriction and shivering
Effect on Effector Mechanisms
- Impairs vasoconstriction and shivering at the blocked spinal levels
- Hence, once triggered, thermoregulatory mechanisms are less effective
Pattern of Hypothermia
Phase 1
- Similar to GA, rapid reduction in core temperature, resulting from redistribution of heat from core to periphery
- Usually, not quite as severe (0.5 - 1C)
Phase 2
- Similar to GA, heat loss > heat production
Phase 3
- Unlike GA, core temp does not necessarily plateau
- Vasoconstriction in the lower limbs - which constitute the bulk of the peripheral thermal compartment - is impaired and metabolic heat cannot be constrained to the core thermal compartment
Combined Spinal and General Anaesthesia
- The threshold to trigger vasoconstriction is 1C lower than with GA alone
- Prevents plateau in core temperature in Phase 3
Neonates vs Adults
Neonates and Thermal Stress
- Susceptible to thermal stress because
- large surface area to volume ratio
- thin subcutaneous tissue
- inability to shiver (not effective in children until a few years old)
- limited sweating ability
- limited ability to control personal environment
- Heat loss due to evaporation when wet is large, eg at birth
- Higher metabolic rate compared to adults (per kg)
- Brown fat and non-shivering thermogenesis is more important in neonates
Monitoring and Maintaining Temperature During Anaesthesia
Sites of Temperature Monitoring
Blood
- Thermistor attached to a pulmonary flotation catheter (Schwan-Ganz catheter).
- Measuring blood temperature in the pulmonary circulation is the best estimate of core temperature but this is a very invasive technique.
- It can also be used to measure cardiac output using thermodilution.
Nasopharynx
- The temperature probe gives a fairly accurate measurement of core temperature and should be positioned just behind the soft palate.
- Incorrect placement leads to inaccurate results due to the cooling effects of inspired gasses.
- Less accurate compared to the oesophageal probe.
Oesophagus
- The probe is most accurate in the lower 25% of the oesophagus.
- When correctly placed it provides a good estimate of cardiac temperature.
- These probes lose their accuracy during thoracotomy, due to local cooling effects of tissues.
Rectum
- Rectal temperature is influenced by the cooling effect of blood returning from the lower limbs and the heat generated by the thermogenic gut flora.
- The insulating effect of faeces results in rectal temperature being 0.5-1.0° C higher than core temperature
- Response time is slow.
Bladder
- Bladder temperature is determined primarily by urine flow and high flow rates are necessary for the bladder temperature to reflect core temperature.
- Low urinary flow makes bladder temperature difficult to interpret in relation to true core temperature.
Warming Devices
- It is generally accepted that no single technique is superior in combating hypothermia. The best results are achieved by combining methods. The costs, risks, and benefits of warming should be considered for each patient, factoring in preexisting medical conditions and the surgical procedure.
- Devices
- Forced air warmers
- Passive coverings
- HME filters
- Fluid warmers
Hazards Related to Patient Warming
- Softened Tracheal Tube
- Infection
- Possible bacterial dissemination by forced-air devices.
- Studies indicate that there is no increased risk associated with forced-air warming devices.
- Burns
- Increased Transcutaneous Medication Uptake
- Hemolysis
- Blood may hemolyze if overheated. If water from a fluid-warming system leaks into blood, hemolysis may result.
- Current Leakage
- Liquid bath and dry heat exchangers must be well grounded. They can leak electrical current into the fluid path.
- Air Embolism
- A hazard with fluid warmers is the possibility of infusing air into the patient, as a result of bubbles created on warming the fluid (outgassing), air entrained through an infusion system, or by delivering air contained in the fluid source. The danger is greatest with pressure infusers, when fluids are infused by a pump, and when rapid, high-volume fluid administration is necessary.
- Interference with Bispectral Index Monitoring
- Falsely elevated bispectral index values have been reported in patients receiving forced-air warming around the head.